Disease
Diverticular Disease of the Colon
People over 80 years of age have
colonic diverticulosis in 75% of cases.
Colon Diverticular Disease
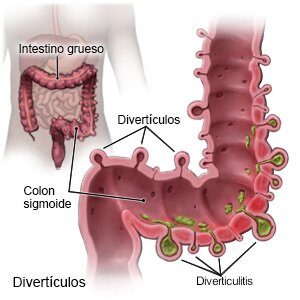
Colonic diverticulosis is the presence of one or more diverticula in the colon. Most diverticulosis is asymptomatic, although in 20% of cases it presents symptoms or becomes complicated causing abdominal pain due to inflammation or bleeding.
A colonic diverticulum is a sac-like pouch of colonic mucosa and submucosa that protrudes through the wall of the colon. Although it can occur in any part of the colon (large intestine), they are mostly located in the left colon or sigma.
The incidence of diverticulosis increases with age. People over 80 years of age have colonic diverticulosis in 75% of cases.
The origin of colonic diverticulosis is not fully understood and appears to have several causes. Studies indicate a correlation between symptomatic diverticular disease and environmental and lifestyle factors, such as a diet low in fiber or rich in red meat, sedentary lifestyle, obesity, smoking and the use of certain drugs (non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids and opiates). Other possible risk factors include hereditary factors and alterations in the structure and motility of the colonic wall.
The diagnosis of diverticulosis is mainly made by colonoscopy, barium enema or CT scan.
Asymptomatic diverticulosis does not require treatment.
When diverticulosis becomes complicated
it can lead to
– Acute diverticulitis, which is the inflammation of a diverticulum, with varying severity, from uncomplicated acute diverticulitis , in which a phlegmon of the intestinal wall occurs, to complicated acute diverticulitis, with formation of an abscess or fistula or even perforation of the colon with peritonitis. The main symptom of diverticulitis is abdominal pain, usually focused in the lower left quadrant of the abdomen.
– Diverticular bleeding (the most common cause of lower gastrointestinal bleeding).
– Segmental colitis associated with diverticular disease.
– Uncomplicated symptomatic diverticular disease, with presence of non-specific digestive symptoms, such as abdominal pain or distension, diarrhea or constipation in patients with diverticulosis in the absence of overt colitis or diverticulitis.
Diagnosis and Treatment
The diagnosis of acute diverticulitis is made by an abdominopelvic CT scan.
Treatment of acute diverticulitis varies according to its severity. In mild cases it can be treated on an outpatient basis with a liquid diet and analgesia and/or oral antibiotics. In more severe cases it requires hospital admission, with digestive rest, serum therapy and intravenous antibiotic treatment. On certain occasions it may require drainage of an intra-abdominal abscess guided by X-ray.
Approximately 15-20% of people admitted for acute diverticulitis require intervention during the same admission, either because of suspected peritonitis on admission or days later, due to poor evolution after starting conservative treatment.
After suffering an episode of acute diverticulitis, resolved by medical treatment (non-surgical), a colonoscopy is recommended 1.5 to 3 months after the resolution of the episode, to confirm the diagnosis and rule out other pathologies ( colon cancer, colitis due to IBD, etc.).
Diverticulitis that is managed nonsurgically may recur. Between 16 – 42% of cases suffer one or more attacks of recurrent diverticulitis.
After an episode of complicated acute diverticulitis has been managed conservatively, sometimes a programmed colon resection is advised when the risk of further potentially serious episodes is considered to be high.
In the case of uncomplicated acute diverticulitis, surgery is generally not indicated, unless the episodes are very repetitive. The most recent guidelines advise assessing each case individually in order to adapt the treatment to the circumstances and specific clinical condition of each patient.
Frequently Asked Questions
about Pilonidal Sinus
- Reddening of the skin
- Pain
- Presence of pus or blood in an opening of the skin.
- Unpleasant odor of oozing pus.
This pathology should be treated by a specialist in coloproctology, which is responsible for the diagnosis and treatment of diseases of the colon, rectum and anus.
As we know, the pilonidal cyst is located in the region above the intergluteal fold, an area of treatment for this specialist.



